Infant Data
Results
INDICATIONS
- Acute cardiovascular collapse: Short-term use for treatment of systemic hypotension. Despite the widespread use of EPINEPHrine/adrenaline during resuscitation, no placebocontrolled studies have evaluated either the tracheal or intravenous administration of EPINEPHrine at any stage during cardiac arrest in human neonates. Nonetheless, it is reasonable to continue to use EPINEPHrine when adequate ventilation and chest compressions have failed to increase the heart rate to greater than 60 beats per minute . The American Heart Association (AHA) did not review the use of EPINEPHrine in the 2015 Neonatal Resuscitation guidelines; therefore, the 2011 AHA and AAP guidelines still apply. Delayed administration of epinephrine during an in-hospital cardiac arrest with an initial nonshockable rhythm was associated with decreased chance of survival to hospital discharge, decreased chance of return of spontaneous circulation, decreased survival at 24 hours, and decreased survival to hospital discharge with a favorable neurological outcome in a retrospective analysis of registry data (n=1558; median age, 9 months; interquartile range, 13 days to 5 years).
- Bronchiolitis:: Adrenergic agents are not recommended for the routine treatment of bronchiolitis in infants and children. Although no evidence supports this use, epinephrine as rescue therapy in rapidly deteriorating patients may have potential.
- Hypotension or Persistent Bradycardia; Prevention of Cardiac Arrest: A pre-arrest small dose may avert cardiac arrest and allow time to treat an acute critical problem or to initiate extracorporeal life support without requiring extracorporeal cardiopulmonary resuscitation for hypotension or persistent bradycardia with a pulse in a patient with an atrisk myocardium. Two retrospective studies demonstrated significant increases in mean arterial blood pressure, systolic blood pressure, and heart rate during acute episodes of hypotension in critically ill children administered low-dose EPINEPHrine boluses at median doses of 0.7 mcg/kg IV (interquartile range (IQR) 0.3 to 2 mcg/kg)and 1.3 mcg/kg IV (range, 0.2 to 5 mcg/kg). The median age was 9 years (IQR, 1 to 15 years) in one study (n=19 patients; 24 episodes). In the other study (n=144), the age groups were younger than 1 year (gestational age 37 weeks or longer) (47%), 1 to 5 years (17%), 5 to younger than 12 years (15%), and 12 to younger than 18 years (22%). Other terms used for this treatment was low-dose, dwindle dose, push-dose pressor, bolus-dose, spritzer vasopressor, or pre-arrest bolus dilute EPINEPHrine
- Severe Sepsis and Septic Shock:
 There was no difference between epinephrine and dopamine for fluid-refractory septic shock in a randomized, double-blind controlled trial (n=40) in India; however, the study was underpowered. After persistent shock despite 2 boluses of normal saline 10 mL/kg, epinephrine 0.2 mcg/kg/min or dopamine 10 mcg/kg/min were started. Doses were increased, if needed, after 15 minutes to epinephrine 0.3 mcg/kg/min or dopamine 15 mcg/kg/min; then again, if needed, after another 15 minutes to epinephrine 0.4 mcg/kg/min or dopamine 20 mcg/kg/min. The mean gestational age was 30.3 weeks (1.1 kg birth weight) for epinephrine group and 30.7 weeks (1.181 kg birth weight) for dopamine group.
There was no difference between epinephrine and dopamine for fluid-refractory septic shock in a randomized, double-blind controlled trial (n=40) in India; however, the study was underpowered. After persistent shock despite 2 boluses of normal saline 10 mL/kg, epinephrine 0.2 mcg/kg/min or dopamine 10 mcg/kg/min were started. Doses were increased, if needed, after 15 minutes to epinephrine 0.3 mcg/kg/min or dopamine 15 mcg/kg/min; then again, if needed, after another 15 minutes to epinephrine 0.4 mcg/kg/min or dopamine 20 mcg/kg/min. The mean gestational age was 30.3 weeks (1.1 kg birth weight) for epinephrine group and 30.7 weeks (1.181 kg birth weight) for dopamine group.
ADVERSE EFFECTS
Compared to dopamine, continuous infusions at doses yielding similar changes in blood pressure are more likely to cause hyperglycemia, tachycardia, and elevations in serum lactate. Cardiac arrhythmias (PVCs and ventricular tachycardia) are also more likely. Renal vascular ischemia may occur at higher doses. Bolus doses are associated with severe hypertension and intracranial hemorrhage. Increased myocardial oxygen requirements. IV infiltration may cause tissue ischemia and necrosis. Suggested treatment: Inject a 1 mg/mL solution of phentolamine into the affected area. The usual amount needed is 1 to 5 mL, depending on the size of the infiltrate.
ADMINISTRATION
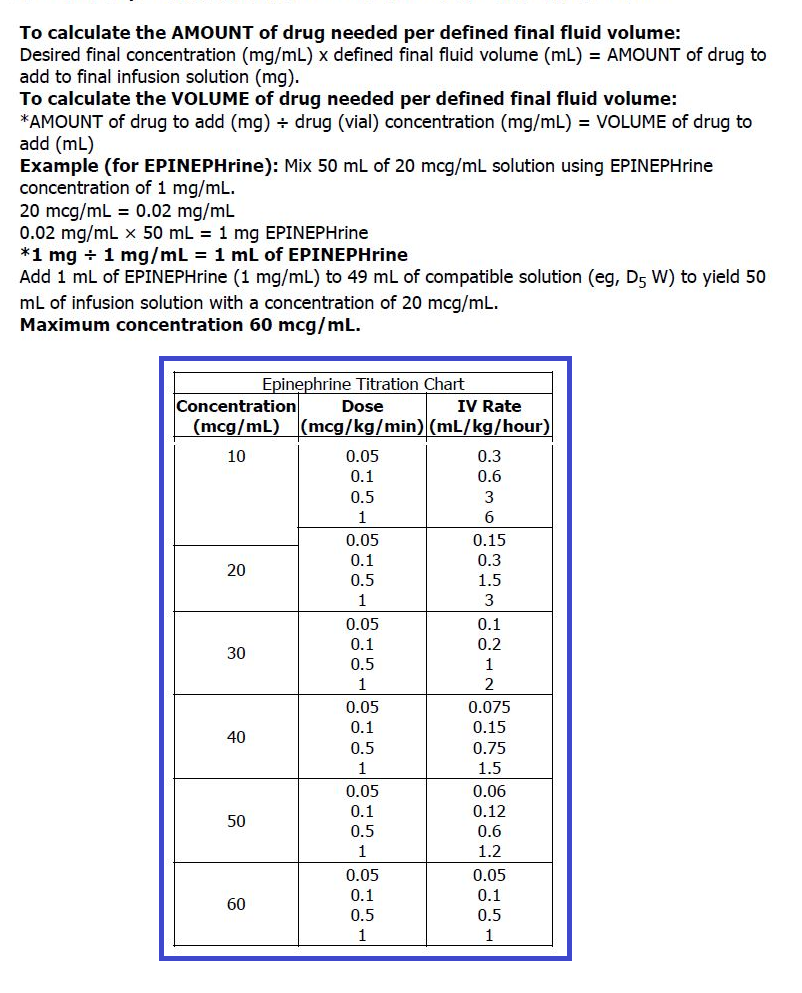
- Intravenous: When giving IV push, follow administration with 0.5 to 1 mL flush of normal saline. Always use the 0.1 mg/mL concentration for individual doses and the 1 mg/mL concentration to prepare continuous infusion solution. For continuous infusion, 10 mcg/mL is the recommended concentration for neonates. Some institutions use standard concentrations of 10, 16, 20, 32, 40, 50, 60, 64, 100, 200, or 700 mcg/mL for continuous infusions in pediatric patients
- Endotracheal: Instill directly into ET tube and follow with several positive-pressure ventilations.
- IV Low-dose EPINEPHrine: Concentrations of 0.01 mg/mL (10 mcg/mL) may be used; via central administration. Preparation (10 mcg/mL): Draw up 9 mL of normal saline into a 10 mL syringe, then draw up 1 mL of EPINEPHrine 0.1 mg/mL.
- Intravenous infusion:
Solution Preparation Calculations
MONITORING
Monitor heart rate and blood pressure continuously. Observe IV site for signs of infiltration. For a full-term newborn, the target heart rate and perfusion pressure (mean arterial pressure minus central venous pressure) are 110 to 160 beats/min and 55 mm Hg, respectively.
